FODMAPs feed your gut microbiome, but that’s not always a good thing. If you have irritable bowel syndrome (IBS) or inflammatory bowel disease, foods high in FODMAPs may be causing your symptoms to flare up.
The low-FODMAPs diet is popular among people with IBS, Crohn’s disease, and ulcerative colitis. In some cases, it’s the only way people find relief from their symptoms.
Read on to learn the benefits of low-FODMAPs diets, who should consider them, how to get started, and what to do if reducing FODMAPs doesn’t help your symptoms.
What are FODMAPs?
FODMAPs are a type of dietary fiber that feeds your gut microbiome. The acronym stands for Fermentable Oligo-, Di-, Mono-saccharides And Polyols.”
The main sources of FODMAPs are processed foods with ingredients like inulin, corn fiber, soy fiber, guar gum, pectin, and sorbitol. However, they also occur naturally in certain fruits and veggies.
FODMAPs are prebiotic, meaning they promote the growth of gut bacteria. While this can be a good thing if you have a healthy microbiome, this form of fiber can also encourage harmful bacterial growth if your gut bacteria are out of balance.
What is a Low-FODMAPs Diet?
Unsurprisingly, the low-FODMAPs diet is all about reducing your intake of FODMAPs. Unlike the majority of diets, low-FODMAPs isn’t for the purpose of weight loss, and it’s certainly not appropriate for everyone.
People with certain gastrointestinal issues or poor digestion sometimes use a low-FODMAPs approach to reset their gut bacteria and reduce their symptoms.
On the low-FODMAPs diet, you simply eliminate high-FODMAPs foods and eat low-FODMAPs alternatives instead. Basically, it’s a matter of knowing which foods and ingredients to avoid, plus reading every food label carefully.
Not everyone has the knowledge or attention to detail to go low-FODMAPs by themselves, so it may be necessary to consult a nutritionist, dietitian, or gastroenterologist for help.
Benefits of a Low-FODMAPs Diet
IBS (Irritable Bowel Syndrome)
Irritable bowel syndrome (IBS) is a disorder that mainly affects the large intestine. Up to 15% of people in industrialized nations have IBS, and women have it twice as often as men[*][*]. It’s the most commonly diagnosed gastrointestinal disorder[*].
The primary symptoms of IBS are abdominal pain and discomfort paired with diarrhea or constipation, or all of the above. Other symptoms include bloating, cramping, and malabsorption of nutrients.
Research shows that IBS patients’ gut bacteria are out of balance, and too much fiber can worsen the situation[*]. That’s why a full 75% of people with IBS get at least some relief from their symptoms by following a low FODMAP diet[*].
Other treatment options include prescription drugs and other dietary changes, but nothing works as well for IBS as a low-FODMAPs diet.
Crohn’s Disease
Crohn’s disease is a type of inflammatory bowel disease (IBD), not to be confused with IBS. It causes inflammation or your digestive tract, often spreading deep into bowel tissues. Different people are affected in different parts of their GI tract.
Symptoms of Crohn’s include abdominal pain, severe diarrhea, fatigue, weight loss, and malnutrition.
About 2 out of every 1000 people have Crohn’s disease, and women are more likely to have it than men[*].
There’s no known cure for Crohn’s disease. Currently, the best outcome is remission, meaning the condition goes dormant and symptoms disappear for long periods of time.
Research shows that the rapid fermentation of FODMAPs creates conditions in the large intestine that may lead to the development of Crohn’s disease[*]. While this makes a low-FODMAPs diet a promising possibility for Crohn’s, there’s not much research yet.
However, a small study of 72 patients with inflammatory bowel disease did find that over half of them experienced significant improvement of symptoms like pain, bloating, gas, and diarrhea by adopting a low-FODMAPs diet for three months[*].
Ulcerative Colitis
Like Crohn’s disease, ulcerative colitis is also a type of inflammatory bowel disease.
The symptoms of ulcerative colitis tend to develop over time, not suddenly. Ulcerative colitis causes severe inflammation and ulcers (sores) of the digestive tract, particularly the colon and rectum.
Living with ulcerative colitis can be debilitating, and it can even lead to life-threatening complications. As with Crohn’s disease, there’s no known cure.
About 2.4 out of every 1000 people have ulcerative colitis[*]. Unlike Crohn’s, men are affected by ulcerative colitis more often than women[*].
Unfortunately, the potential benefits of lowering FODMAPs for ulcerative colitis haven’t received much attention from the scientific community yet.
In one study of 32 people with inflammatory bowel disease, large doses of FODMAPs caused flare-ups in their symptoms[*]. This finding highlights the possibility that FODMAPs may worsen symptoms if you have ulcerative colitis, so avoiding them could definitely be beneficial.
Another small study found significant improvement after three months of low-FODMAPs for ulcerative colitis patients, but it lacked a control group[*].
Less Bloating and Fewer Digestive Symptoms
What if you have bloating, or other digestive symptoms like heartburn or nausea, but no diagnosis? These symptoms may affect up to 52% of people, most of whom don’t meet all the criteria for IBS or other gastrointestinal disorders[*].
But just because you don’t have a formal diagnosis doesn’t mean you aren’t suffering!
One cause of bloating and other digestive symptoms is gut dysbiosis. That means imbalanced or impaired microbes. In other words, the little critters in your gut that regulate things like immune balance and even brain function are in trouble.
Gut dysbiosis is also one potential cause of IBS and probably increases the risk of IBD (Crohn’s and ulcerative colitis)[*]. So while each of these problems is different, they may share at least one root cause.
When you add extra FODMAPs on top of gut dysbiosis, it can make the problem worse[*].
Low-FODMAPs diets are very good at dealing with bloating in IBS because they help rebalance the microbiome of people with IBS[*]. Therefore, it stands to reason that in people without IBS who suffer from bloating and related symptoms, low-FODMAPs is worth a try.
At least one small study confirms this idea. The authors of the study put some runners who were suffering exercise-related GI symptoms on a low-FODMAPs diet and found it helped reduce their symptoms[*].
Who is the Low-FODMAPs Diet For?
The low-FODMAPs diet is worth a try if you can’t solve your gastrointestinal symptoms.
However, before you implement a low-FODMAPs approach to eating, you should see a doctor for a diagnosis (or a referral to a specialist) first.
While low-FODMAPs works great in IBS and is promising for IBD and other GI problems, it’s not a magic bullet. If you have another problem–like a food allergy, bowel obstruction, or infection–you’ll be spinning your wheels without addressing the real cause.
Who Should Avoid a Low-FODMAPs Diet?
Your gut microbiome is incredibly complex and delicate. It affects everything from digestion and gut health to the function of your immune system and brain[*].
So it stands to reason that before you try to alter it, you need to have a good reason. If you don’t have any gastrointestinal symptoms, there’s no benefit to going low-FODMAPs, period.
Prebiotics are generally a good thing. In healthy people without dysbiosis, reducing your intake of prebiotic fibers might actually lead to imbalances in gut bacteria[*][*].
If you have low-grade symptoms but haven’t been diagnosed with IBS or IBD, it may be wiser to begin with an elimination diet (where you eliminate foods like wheat and dairy for a time) or try probiotics before you consider low FODMAPs.
How to Go Low-FODMAPs
Stages of a Low-FODMAPs Diet
If you decide to try a low-FODMAPs diet to ease your symptoms, you need to understand each of the three phases.
Stage 1: The Strict Elimination Phase
During this phase, you avoid all high-FODMAPs foods (see High-FODMAPs Foods to Avoid).
The strict elimination period usually lasts 8-12 weeks, and most people notice improvements in their symptoms within a few days to a few weeks.
Stage 2: The Gradual Reintroduction Phase
After several months of strict elimination, it’s time to reintroduce FODMAPs gradually. As with other elimination diets, the purpose of this phase is to determine which foods and which types of FODMAPs cause your symptoms to flare up.
Some people may discover that all FODMAPs are a problem, while others will narrow it down to specific foods or food groups.
The key during gradual reintroduction is not to rush it. Add back one or two foods per week so you can get an accurate picture of what the effects are, and if you determine that a specific food causes symptoms, eliminate it and move on.
Stage 3: The Modified Low-FODMAPs Diet
Once you complete the gradual reintroduction phase, you should have a clear idea of the exact foods and ingredients that cause your symptoms to flare up. The modified low-FODMAPs diet is a personalized diet that excludes or limits these problem foods so your body can continue to heal.
While it may be tempting to permanently eliminate all FODMAPs if you obtained relief during the strict elimination phase, that’s probably not a good idea. There’s evidence that for people with IBS and IBD, low or moderate doses of some FODMAPs (which vary from person to person) contribute to gut health and bacterial diversity[*][*].
High-FODMAPs Foods to Avoid
Below you’ll find a complete list of foods and ingredients you need to avoid altogether during the elimination phase of your low-FODMAPs diet.
During the gradual reintroduction phase, you can reintroduce them in any order you like, but we suggest that you reintroduce them in the order of this list–starting with healthy whole foods (like fruits and vegetables) first.
As you reintroduce foods and ingredients, remember to wait 3-4 days or longer before adding the next item(s) back to your diet. That way, you can figure out what’s causing your symptoms.
It’s highly unlikely that you regularly eat all the foods on this list, so you don’t need to take months and months during the reintroduction phase testing every single item. Instead, you can print the list, then circle the foods you ate on a regular basis before the elimination period.
Vegetables
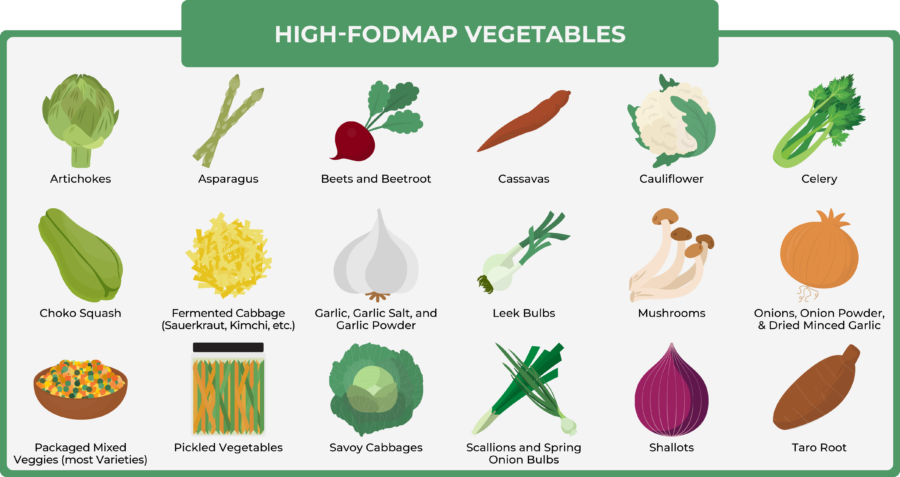
- Artichokes
- Asparagus
- Beets and beetroot
- Cassavas
- Cauliflower
- Celery
- Choko squash
- Fermented cabbage (sauerkraut, kimchi, etc.)
- Garlic, garlic salt, and garlic powder
- Leek bulbs
- Mushrooms
- Onions, onion powder, and dried minced garlic
- Packaged mixed veggies (most varieties)
- Pickled vegetables
- Savoy cabbages
- Scallions and spring onion bulbs
- Shallots
- Taro root
Fruits
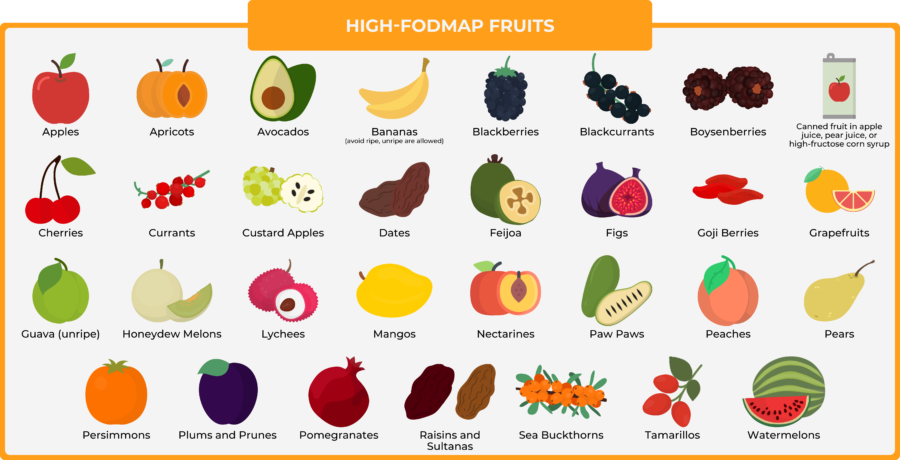
- Apples
- Apricots
- Avocados
- Bananas (avoid ripe, unripe are allowed)
- Blackberries
- Blackcurrants
- Boysenberries
- Canned fruit in apple juice, pear juice, or high-fructose corn syrup
- Cherries
- Currants
- Custard apples
- Dates
- Feijoa
- Figs
- Goji berries
- Grapefruits
- Guava (unripe)
- Honeydew melons
- Lychees
- Mangos
- Nectarines
- Paw paws
- Peaches
- Pears
- Persimmons
- Plums and prunes
- Pomegranates
- Raisins and sultanas
- Sea buckthorns
- Tamarillos
- Watermelons
Meats
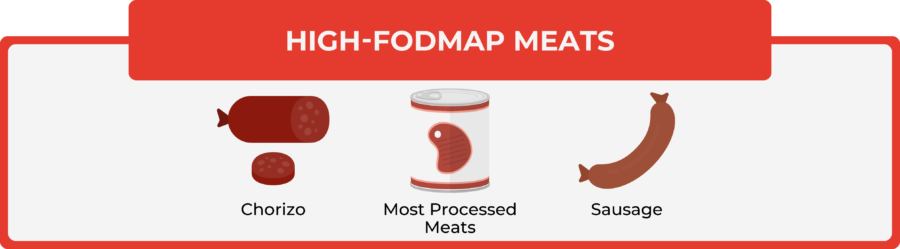
- Chorizo
- Most processed meats (check the ingredients list)
- Sausage
Dairy Products
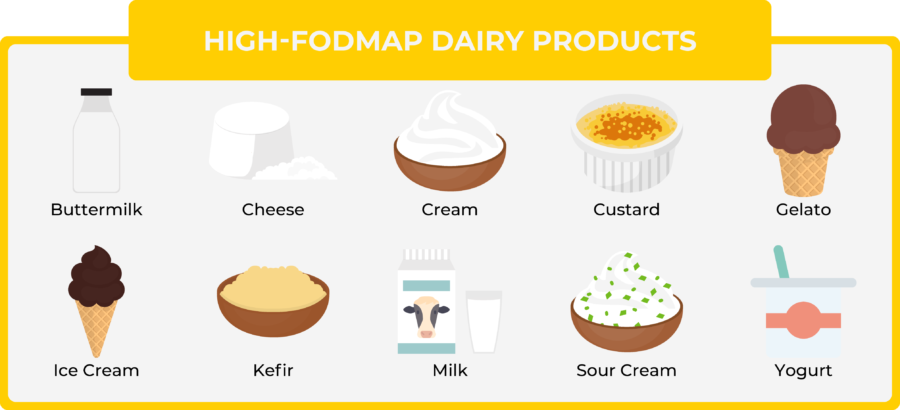
- Buttermilk
- Cheese (especially cottage, cream, Halmoumi, and ricotta)
- Cream
- Custard
- Gelato
- Ice cream
- Kefir
- Milk (cow, evaporated, goat, sheep)
- Sour cream
- Yogurt
Beverages
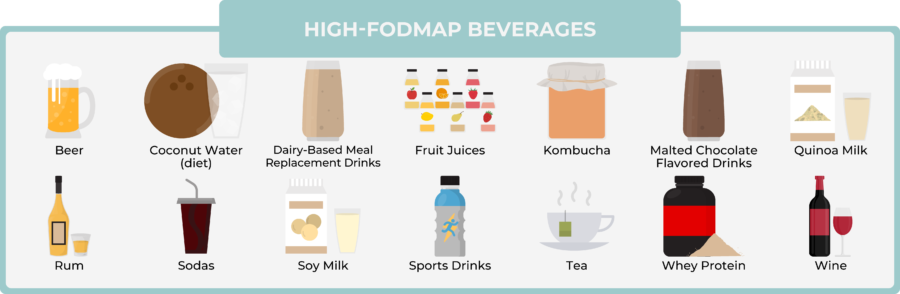
- Beer
- Coconut water
- Dairy-based meal replacement drinks (Ensure, SlimFast, etc.)
- Fruit juices (especially apple, mango, orange, pear, raspberry, and strawberry)
- Kombucha
- Malted chocolate flavored drinks
- Quinoa milk
- Rum
- Sodas, especially with HFCS
- Soy milk
- Sports drinks
- Tea (chai, chamomile, dandelion, fennel, fruit, herbal, oolong
- Whey protein (hydrolyzed and concentrate, unless lactose-free)
- Wine
Legumes
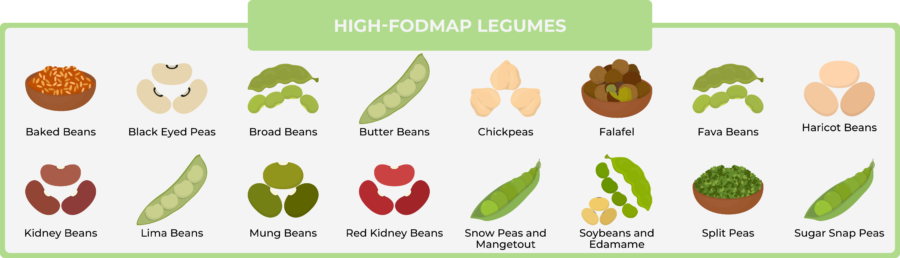
- Baked beans
- Black eyed peas
- Broad beans
- Butter beans
- Chickpeas
- Falafel
- Fava beans
- Haricot beans
- Kidney beans
- Lima beans
- Mung beans
- Red kidney beans
- Snow peas and mangetout
- Soybeans and edamame
- Split peas
- Sugar snap peas
Sauces, Sweeteners, and Condiments

- Agave
- Carob powder
- Caviar
- Fructose
- Fruit bars
- Glucose-fructose syrup
- Gravy with onions
- High fructose corn syrup (HFCS)
- Honey
- Hummus
- Inulin
- Isomalt
- Jelly or jam (especially with strawberries, mixed berries, or HFCS)
- Lactitol
- Maltitol
- Mannitol
- Molasses
- Pesto sauce
- Pickle or vegetable relish
- Quince paste
- Sorbitol
- Stock cubes
- Sugar-free sweets containing polyols (ending in -ol)
- Tahini
- Tzatziki sauce
- Xylitol
Wheat and Wheat Products

- Biscuits
- Bread
- Breadcrumbs
- Breakfast cereals
- Cakes
- Cereal bars
- Cookies
- Croissants
- Crumpets
- Dinner rolls
- Egg noodles
- Einkorn
- Flour
- Gnocchi
- Muffins
- Noodles
- Pasta
- Pastries
- Semolina
- Spelt
- Tortillas
- Udon noodles
- Wheat bran
- Wheat germ
Other Grains
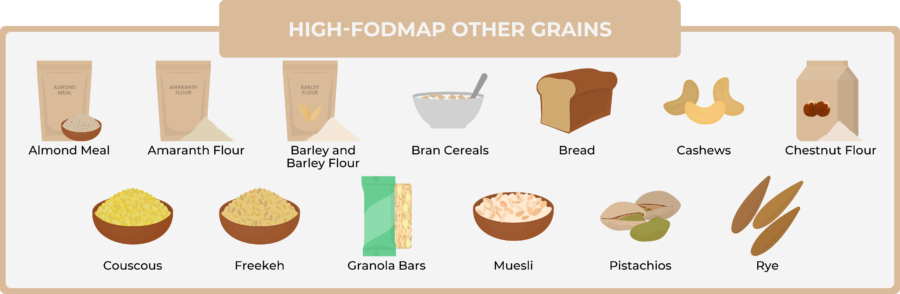
- Almond meal
- Amaranth flour
- Barley and barley flour
- Bran cereals
- Bread
- Cashews
- Chestnut flour
- Couscous
- Freekeh
- Granola bars
- Muesli
- Pistachios
- Rye
High-FODMAPs Ingredients in Processed Foods
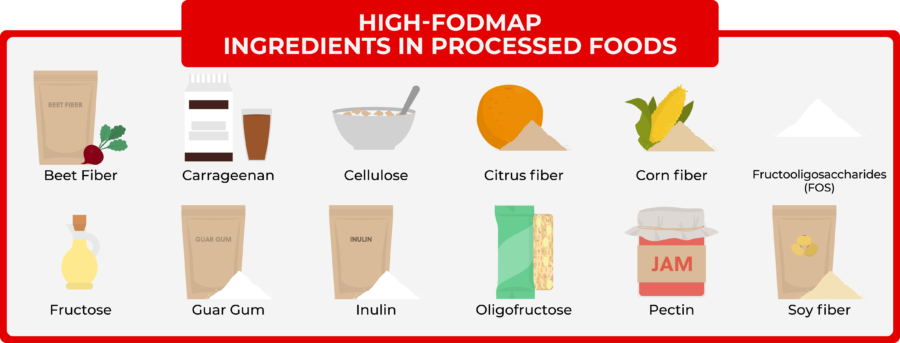
- Beet fiber
- Carrageenan
- Cellulose
- Citrus fiber
- Corn fiber
- Fructooligosaccharides (FOS)
- Fructose
- Guar gum
- Inulin
- Oligofructose
- Pectin
- Soy fiber
Low-FODMAPs Foods to Eat Instead
Now that you know what to avoid, you may be wondering: what can I eat on a low FODMAPs diet?
Fortunately, you can still eat plenty of foods. Print this list out and take it to the grocery store so you can match your choices to approved low FODMAPs foods.
Animal Products
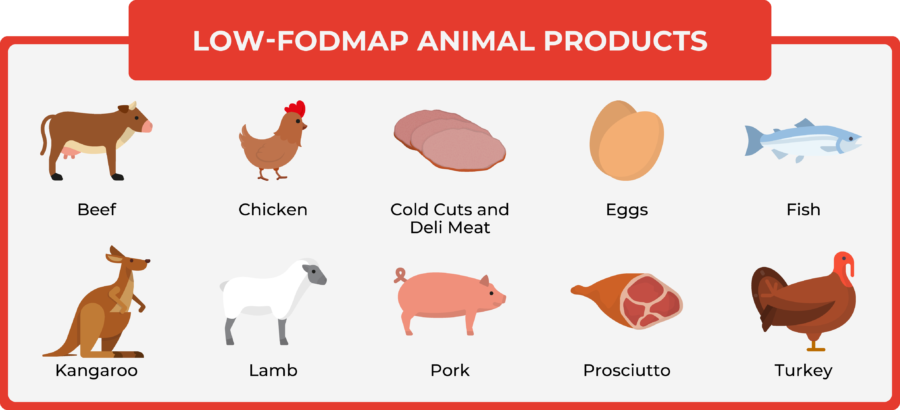
- Beef
- Chicken
- Cold cuts and deli meat (e.g., ham and turkey breast, but check ingredients)
- Eggs
- Fish
- Kangaroo
- Lamb
- Pork
- Prosciutto
- Turkey
Fats, Oils, Nuts, and Seeds
- Macadamia nuts
- Pine nuts
- Sesame seeds
- All fats and oils are allowed
- Recommended fats:
- Butter
- Extra virgin olive oil
- Extra-virgin coconut oil (cold-pressed)
- Ghee
Condiments, Herbs, and Spices
Most herbs and spices are allowed (check ingredients)
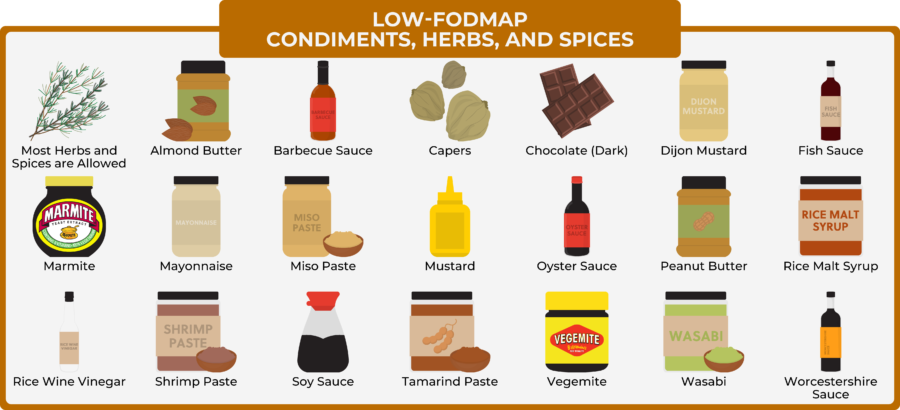
- Almond butter
- Barbecue sauce (check ingredients carefully)
- Capers
- Chocolate (dark)
- Dijon mustard
- Fish sauce
- Marmite
- Mayonnaise (without garlic or onion listed on label)
- Miso paste
- Mustard
- Oyster sauce
- Peanut butter
- Rice malt syrup
- Rice wine vinegar
- Shrimp paste
- Soy sauce
- Tamarind paste
- Vegemite
- Wasabi
- Worcestershire sauce
Vegetables
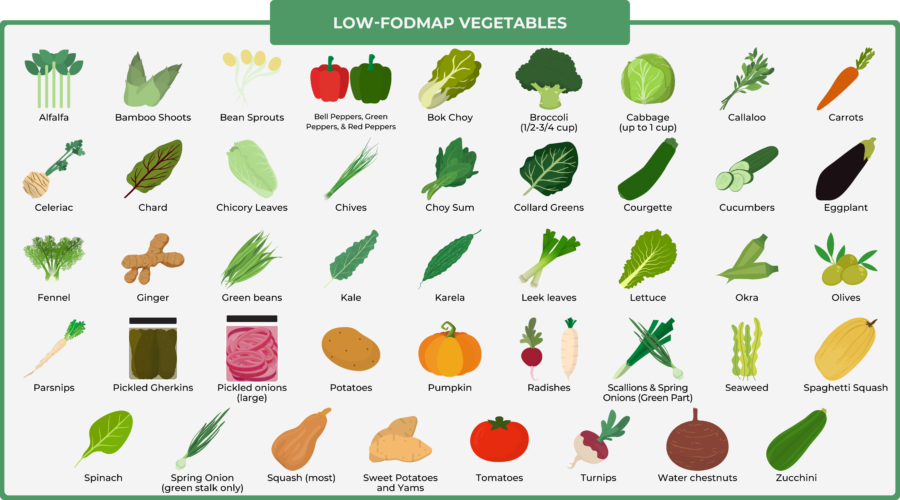
- Alfalfa
- Bamboo shoots
- Bean sprouts
- Bell peppers, green peppers, and red peppers
- Bok choy
- Broccoli (1/2-3/4 cup)
- Cabbage (up to 1 cup)
- Callaloo
- Carrots
- Celeriac
- Chard
- Chicory leaves
- Chives
- Choy sum
- Collard greens
- Courgette
- Cucumbers
- Eggplant
- Fennel
- Ginger
- Green beans
- Kale
- Karela
- Leek leaves
- Lettuce (butter, iceberg, radicchio, red coral, rocket, romaine, cos)
- Okra
- Olives
- Parsnips
- Pickled gherkins
- Pickled onions (large)
- Potatoes
- Pumpkin
- Radishes
- Scallions and spring onions (green part)
- Seaweed
- Spaghetti squash
- Spinach
- Spring onion (green stalk only)
- Squash (most)
- Sweet potatoes and yams
- Tomatoes
- Turnips
- Water chestnuts
- Zucchini
Fruits
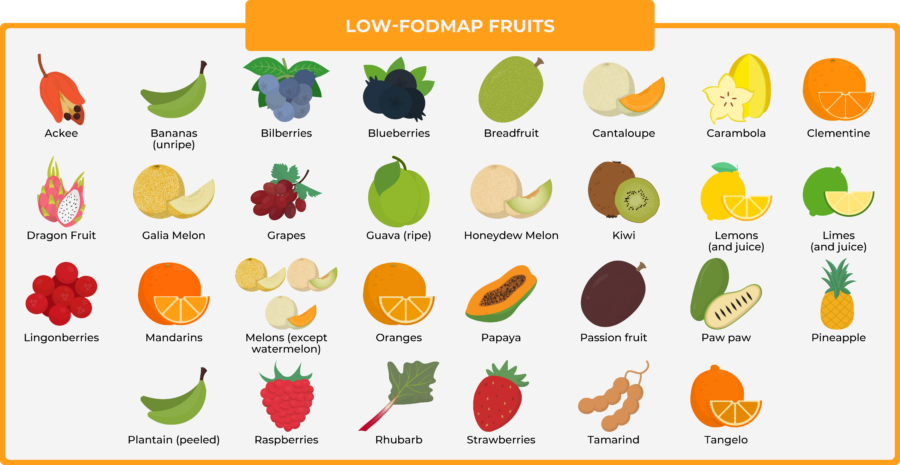
- Ackee
- Bananas (unripe)
- Bilberries
- Blueberries
- Breadfruit
- Cantaloupe
- Carambola
- Clementine
- Dragon fruit
- Galia melon
- Grapes
- Guava (ripe)
- Honeydew melon
- Kiwi
- Kiwifruit
- Lemons (and juice)
- Limes (and juice)
- Lingonberries
- Mandarin
- Mandarins
- Melons (except watermelon)
- Orange
- Papaya
- Passion fruit
- Passionfruit
- Paw paw
- Pineapple
- Plantain (peeled)
- Raspberries
- Rhubarb
- Strawberries
- Tamarind
- Tangelo
Beverages

- Almond milk
- Clear spirits (vodka, gin, etc.)
- Coffee
- Egg protein powder
- Green tea
- Hemp milk
- Kvass
- Lactose free milk
- Macadamia milk
- Rice protein powder
- Water
- Whey protein isolate
- Whiskey
Dairy Products
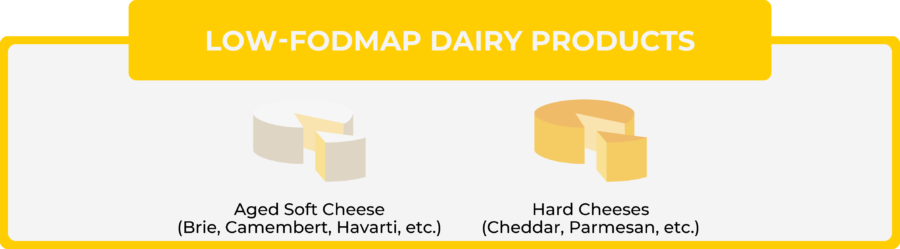
- Aged soft cheese (Brie, camembert, havarti, etc.)
- Hard cheeses (cheddar, parmesan, etc.)
Grains
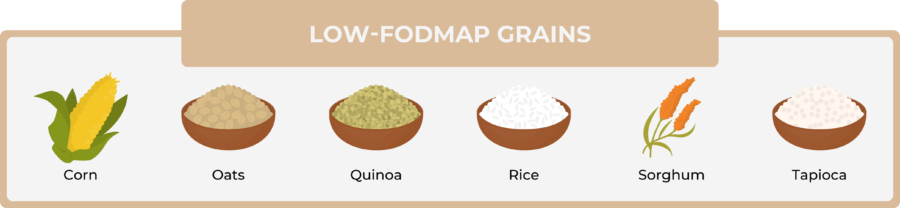
- Corn
- Oats
- Quinoa
- Rice
- Sorghum
- Tapioca
Sweeteners
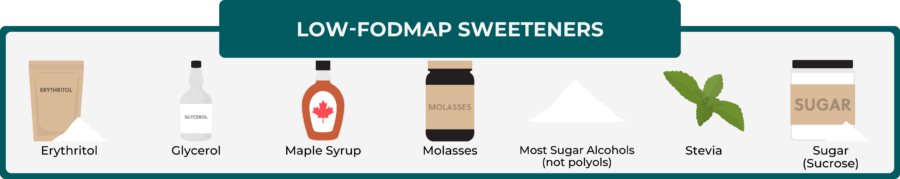
- Erythritol
- Glycerol
- Maple syrup
- Molasses
- Most sugar alcohols (not polyols)
- Stevia
- Sugar (sucrose)
Low FODMAPs and The Ketogenic Diet
Low FODMAPs and the ketogenic diet are two entirely different diets, with different purposes.
However, they’re also 100% compatible. If you’re already on the keto diet, it’s actually easier to go low FODMAPs.
If you have a keen eye, you may have noticed that over 75% of the foods on the “High-FODMAPs Foods to Avoid” list are already excluded from the keto diet approved foods list.
So if you’re currently on the keto diet and decide to go low-FODMAPs, you’ll have a significant advantage because you won’t have to work as hard to eliminate foods.
That said, if you aren’t on the keto diet yet and are considering going low-FODMAPs, you should probably eliminate FODMAPs before you go keto. That’s because it’s already complicated to eliminate FODMAPs, and starting the keto diet has its own set of challenges (and rewards).
If you go low-FODMAPs first, you can always go keto later on. Because you avoid processed foods on keto and eat real foods instead, it’s easy to combine keto with a low FODMAPs approach to enjoy the many benefits of keto.
What if Low FODMAPs Doesn’t Work for Me?
Although a low FODMAPs diet works for up to 75% of IBS patients, that still leaves 25% of people who don’t respond to it at all. And while there isn’t data for ulcerative colitis or Crohn’s, it’s safe to say that it doesn’t work for 100% of people with IBD, either.
Luckily, you’ve got other options to consider if you don’t get relief by eliminating FODMAPs:
- Food allergy tests
- An elimination diet
- A chemical-free diet
- Stress reduction
Low FODMAPs diets don’t address food allergies, so it’s worth getting tested for food allergies if you’re still experiencing symptoms. Often, symptoms are caused by a common allergy to wheat or dairy[*].
Other Diets to Consider
Not all food allergies show up on tests! That’s why an elimination diet can be a smart solution for some people. On an elimination diet, you typically eat from a limited list of foods, then gradually add back potential problem foods.
It works sort of like a low FODMAPs diet, but instead of FODMAPs, you’re eliminating all foods that might cause symptoms. A nutritionist, dietitian, or gastroenterologist can help you plan an elimination diet.
On the other hand, for some people, a chemical-free diet works best to ease GI symptoms[*]. That means eliminating the following ingredients for several months:
- Salicylates
- Amines
- MSG
- Benzoates
- Sulfites
- Nitrites
- Sorbic acid
- Artificial colors
- Artificial sweeteners
If you feel better during this period, that means you’ve found the cause of your symptoms! Optionally you can reintroduce the chemicals one-by-one to figure out the culprit, but honestly, most of these ingredients are worth avoiding, anyway.
Stress Reduction (and Butter)
Now, let’s talk about stress.
Multiple studies show that stress causes stomach discomfort, and it’s also been proven to raise your risk of IBS[*][*][*][*]. So whether or not you use a low-FODMAPs diet or another approach like the elimination diet, reducing and managing your stress levels is essential if you want to feel better.
Finally, another solution that might work to ease your gastrointestinal symptoms is eating more grass-fed butter. Grass-fed butter is high in butyrate, a short-chain fatty acid with stress-reducing properties[*]. People with IBS, IBD, and other GI problems have reduced butyrate levels[*].
If you go keto you can eat all the grass-fed butter you want, and it might help you feel better.
The Bottom Line: Low-FODMAPs Diets Are Worth a Try
If you’re struggling with symptoms but aren’t sure of the cause, talk to your doctor and ask for a referral to a gastroenterologist if needed. You need to be certain of the cause rather than assume.
If you can’t get relief through conventional means, a low-FODMAPs diet is definitely worth a try. It works in up to 75% of people with IBS, and the evidence for IBD and general gastrointestinal symptoms is promising, too[*].
Other effective measures to consider include elimination diets, chemical-free diets, and stress reduction. Some people may need to combine several of these strategies to find relief.
Finally, don’t forget that the ketogenic diet is not only compatible with all of these approaches, it can actually make life easier if you’re already on a restricted diet. Keto automatically eliminates problem foods and replaces them with nutritious alternatives.
Not only that, it also helps address the root causes of gut issues by rebalancing your gut bacteria, reducing inflammation, and lowering insulin levels[*][*][*].
