Following a ketogenic diet can improve gut issues such as excess gas production, bloating, and flatulence (*).
One explanation is that the keto diet is naturally lower in sugar and FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols). FODMAPs are carbs that cause digestive distress in some people. Therefore, avoiding these triggers can help the gut to heal over time (*).
If you’re specifically dealing with SIBO — or more generally, IBS — this guide discusses everything you should know about these conditions and how to use keto properly for your digestive health.
What’s the Relationship Between SIBO, IBS, and Bloating?
SIBO is an acronym for small intestinal bacterial overgrowth. It’s a condition characterized by excessive bacteria in the small intestine and is more common than previously thought, thanks to today’s readily available tests to diagnose SIBO (*).
Note that while everyone has bacteria in their gut, an imbalance or dysbiosis causes problems.
On the other hand, IBS or irritable bowel syndrome (also known as irritable colon), can result from SIBO. Symptoms of IBS like bloating, distension, cramping, constipation, and diarrhea can mimic those of SIBO (*).
Furthermore, SIBO is more common in diarrhea-predominant IBS (IBS-D) than constipation-predominant IBS (IBS-C) (*).
According to a meta-analysis, people with IBS are more likely to have SIBO (*). This means that if you’re diagnosed with IBS, then it’s reasonable to assume that you might have SIBO.
One way to confirm SIBO is through breath testing (*). We’ll discuss more about it, including other testing methods, later in this article. Bloating, on the other hand, is a symptom common to SIBO and IBS. It’s triggered by eating foods containing FODMAPs. Bacteria in your gut feed on these sugars, causing fermentation, gas production, then bloating (*).
In this article, we’ll focus more on SIBO as an underlying cause of IBS, starting with its possible causes.
What Are the Possible Causes of SIBO?
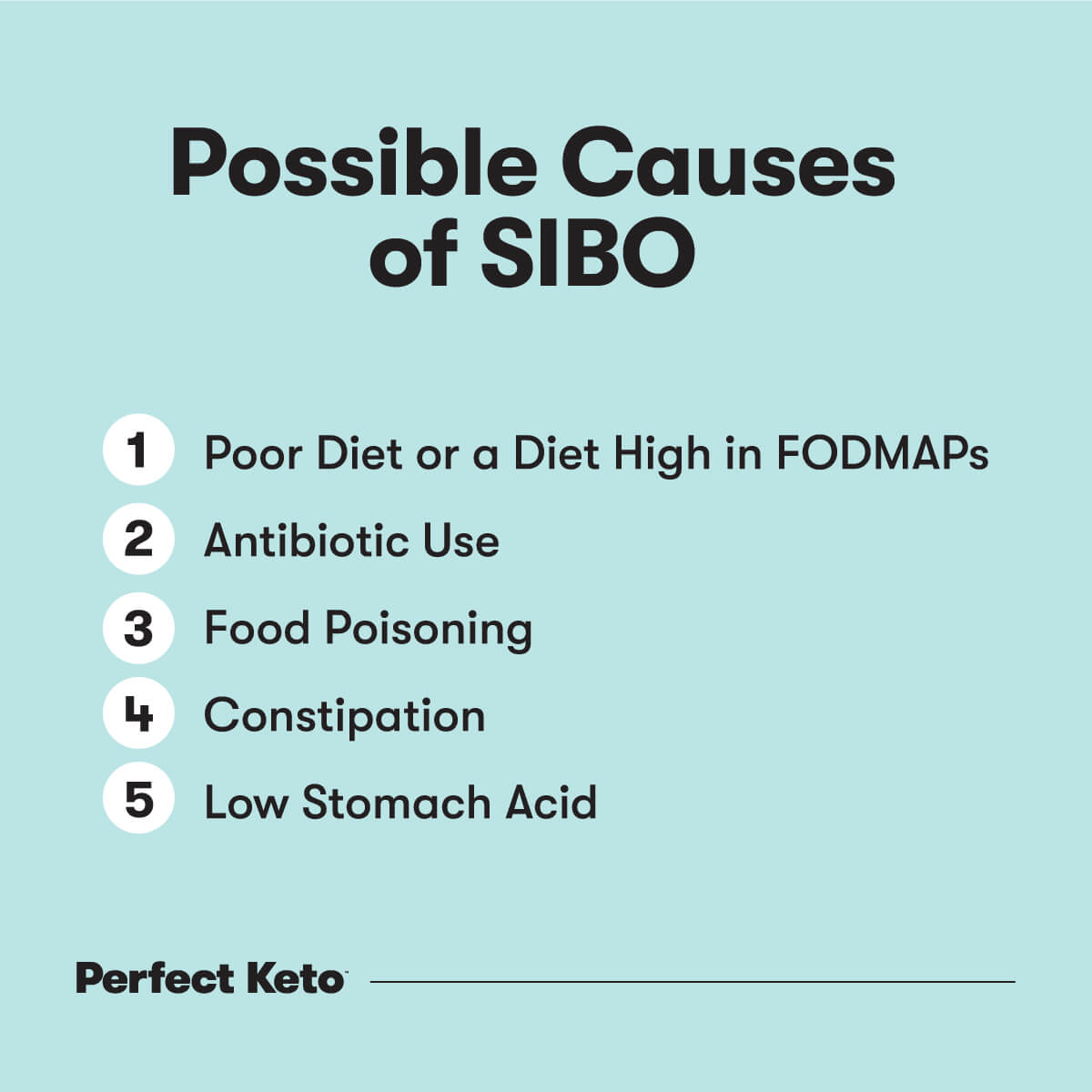
According to various research studies, these factors can increase a person’s risk for bacterial overgrowth:
1. Poor Diet or a Diet High in FODMAPs
A diet that’s rich in carbohydrates and refined sugars may contribute to SIBO.
One study found that obese subjects with SIBO ate more carbs and refined sugars than the subjects without SIBO. Furthermore, they had a low fiber intake (*).
Here are possible explanations behind this:
Too much sugar can change gut bacteria by reducing their diversity, which is linked to dysbiosis (* , *).
Furthermore, excess sugar increases Proteobacteria and decreases Bacteroidetes. While these bacteria are beneficial, an imbalance leads to inflammation.
Certain carbohydrates are more fermentable — FODMAPs. Meaning, they serve as food for gut bacteria. While this isn’t necessarily a bad thing, some people tend to be more sensitive to fermentation and therefore experience gut issues.
Sensitive people should stay away from high FODMAP foods like wheat, barley, and high-fructose fruits like apples and mangoes.
As you may notice, these foods aren’t keto-friendly, to begin with. (However, there are a few keto-friendly foods with FODMAPs you should still be aware of. We’ll show you the foods to avoid later in this article.)
2. Antibiotic Use
Although SIBO can be treated with antibiotics, the long-term use of antibiotics disrupts your gut microbiome.
According to a review article in Frontiers, antibiotics reduce microbiota diversity and can also lead to the overgrowth of pathobionts — these are potentially harmful microorganisms in the gut (*).
The same article also mentioned that early exposure to antibiotics (infants, for example) might lead to the development of inflammatory bowel disease or IBD (*). Note that SIBO is present in some patients with IBD.
While antibiotics benefit us by fighting infection, they do come with side effects — gut microbiome dysbiosis being one.
3. Food Poisoning
Food poisoning, or the irritation of your digestive tract caused by contaminated food, is common in older adults, younger children, and people with a weakened immune system (* , *).
During food poisoning, pathogens throw off the movement of ions and water in your gastrointestinal tract, resulting in diarrhea (*). Study shows that frequent, longer, and severe diarrhea can disrupt the gut microbiome (*).
This is why probiotics are sometimes prescribed by your doctor to stop diarrhea and restore digestive balance (*).
New research suggests that the appendix may serve as a “safe house” for helpful gut bacteria, such as Bacteroides, Lactobacillus, and Bifidobacterium (*). That way, when you get diarrhea from food poisoning, the beneficial microbes in your appendix can repopulate your digestive system.
However, people who’ve had their appendix removed might need to take additional measures to repopulate their good gut bacteria. Taking probiotics and eating fermented foods, for instance.
4. Constipation
Having less frequent bowel movements can also lead to small intestinal bacterial overgrowth. So, if you’re having constipation in addition to related symptoms like abdominal pain and bloating, you have a reason to suspect SIBO.
A 2011 study explained that methanogenic flora in the gut causes excessive methane production, which is often the case in patients with constipation. Data also suggests that methane gas slows gut transit or the time it takes for food to move from the mouth to the end of the large intestine (*).
Since decreased intestinal transit time can increase fermentation, you may want to prevent constipation from happening in the first place. Consuming a high-fat diet that includes dietary fiber promotes regular bowel movement.
5. Low Stomach Acid
Stomach acid or gastric acid contains digestive enzymes that break down food. It also kills microbial pathogens (* , *).
Things get problematic when you have high gastric pH levels. For instance, a weakly acidic pH level of 4.0 increases the risk of bacterial overgrowth (*).
Symptoms of low stomach acid include bloating, burping, abdominal pain, and cramping, which can indicate SIBO. Factors that could lead to low stomach acid levels include H. pylori (which attacks the stomach lining), increased stress, and advancing age (* , *, *, *).
If you’re suspecting low stomach acid, make sure to consult with your doctor for further assessment.
SIBO Symptoms to Note
Most SIBO symptoms are similar to IBS symptoms and they can range from mild to worse. Note for the following(* , *):
- Abdominal pain
- Bloating
- Flatulence
- Nausea
- Diarrhea
- Constipation
Vitamin deficiency resulting from the malabsorption of nutrients is another clinical feature of bacterial overgrowth. Poorly absorbed nutrients include protein, fat, fat-soluble vitamins A, D, E, and K (* , *).
Interestingly, some patients report an increased craving for foods high in sugar and starches (*). This can raise blood sugar levels and cause weight gain.
Should You Get Tested for SIBO?
Diagnostic testing is the best way to confirm whether you have SIBO. Your doctor may order non-invasive breath tests which are popular. Breath tests check for specific gases produced by bacteria in your small intestine, such as hydrogen and methane (*).
Another test is the GI map stool test which looks at specific bacteria, viruses, and other microorganisms. Meanwhile, the jejunal aspiration test is considered the “gold standard” for SIBO diagnosis (*).
Is the Keto Diet Good for SIBO?
Yes. A low-carbohydrate diet such as keto can be very effective for reducing bloating in general, and SIBO in particular. Most people with SIBO find relief in following a low FODMAP diet. Though entirely different from keto, combining a low FODMAP diet with a low-carb eating plan eliminates trigger foods to improve SIBO symptoms.
Common gut offenders (high FODMAP foods) that cause fermentation include apples, pears, grains, cereals, soya beans, dairy products, and polyols or sugar alcohols (*). Note that all these foods are high in carbohydrates except for polyols, which are keto-friendly sweeteners.
So, for someone thinking of going low carb for SIBO management and gut health, on top of other goals like weight loss — the keto diet is a great option.
People struggling with diarrhea-predominant IBS (IBS-D) may also experience symptom improvement by following a very low-carbohydrate diet. In a 2009 study, the participants’ stool frequency decreased while stool consistency went from diarrheal to normal. They also experienced pain relief (*).
How Can I Naturally Get Rid of SIBO?
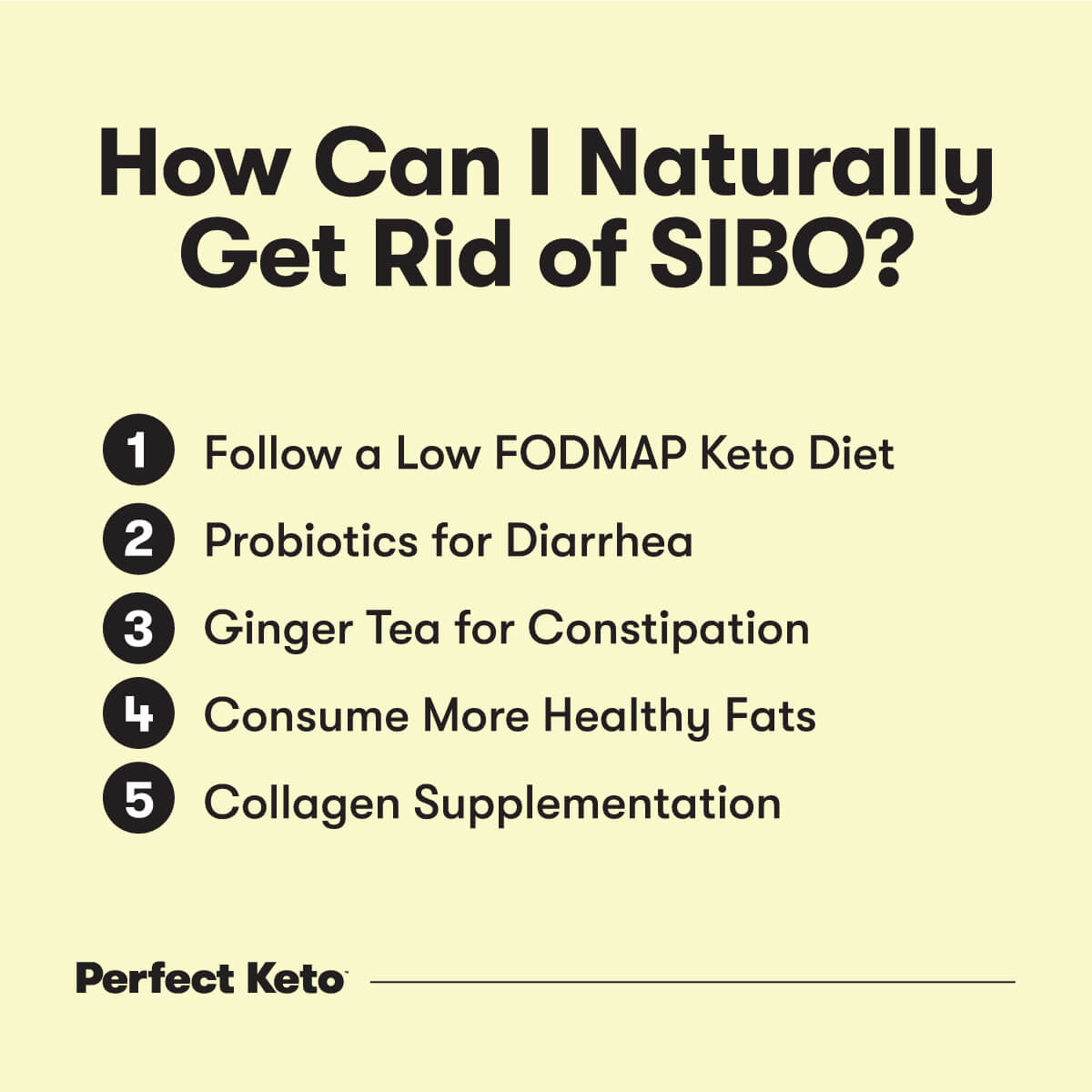
The good news is, SIBO can be treated with natural remedies, such as combining a low FODMAP and low carb diet, taking probiotics, and collagen supplementation. Your doctor may also prescribe antibiotics to reduce bacterial overload.
1. Follow a Low FODMAP Keto Diet
This means doing a very low carb diet, at the same time, avoiding common FODMAPS like:
- Fructans and GOS (galacto-oligosaccharides): onion, garlic, legumes, asparagus, brussels sprouts, broccoli, and cabbage
- Lactose: dairy products such as milk, cheeses, and butter
- Fructose: apples, mangoes, pears, watermelons (note that apples, mangoes, and pears are not keto-friendly fruits to start with.)
- Polyols: sugar alcohols such as xylitol, maltitol, sorbitol, isomalt, and mannitol
Follow this low-carb, low-FODMAP diet for a couple of weeks and pay attention to your symptoms. Once symptoms resolve, you may start reintroducing one food at a time from a FODMAP category. Just make sure you’re not consuming a high-carbohydrate fruit from the ones listed above to avoid getting kicked out of ketosis.
Reintroducing FODMAPs slowly will help you maintain a healthy and diverse gut microbiome. “Numerous microbes help build a good immune system to fight the bacteria and viruses attacking the body. This reduces the chance of allergies, infections, and asthma,” says Isaac Robertson, a nutritionist, personal fitness trainer, and co-founder at Total Shape.
2. Probiotics for Diarrhea
Although studies on probiotics for SIBO are limited, taking probiotics can resolve chronic diarrhea related to bacterial overgrowth and distention.
For instance, one study showed that subjects who took probiotics experienced great reductions in pain, bloating, belching, and diarrhea compared to the subjects who took only antibiotics (*).
Smidge (GutPro) is a good option since it’s free of allergens such as milk, shellfish, and eggs. Furthermore, it doesn’t contain prebiotics that may feed gut bacteria and worsen SIBO symptoms.
3. Ginger Tea for Constipation
People suffering from constipation may find relief by taking ginger tea. Ginger tea can also alleviate IBS symptoms and support a healthy gut.
A 2018 review found that ginger extract improved gastrointestinal motility. Ginger speeds up gastric emptying and stimulates anal contractions in healthy individuals (*).
As an added benefit, ginger may relieve nausea, one of the symptoms of SIBO (*).
4. Consume More Healthy Fats
A keto diet meal plan comprises mostly fats (*). This increased fat intake drives up ketones and causes you to lose weight, and in SIBO cases, it promotes bowel movement in those experiencing constipation.
Fat stimulates motility, and its effect on you might even be greater if you just came from a low-fat, high-carbohydrate diet or a SAD (standard American diet).
Be sure to choose healthy fat sources such as MCT oil, eggs, olive oil, fatty cuts of meat, and avocados.
5. Collagen Supplementation
Collagen is a major component of your body tissues, and it plays a role in promoting gut health.
SIBO can lead to leaky gut or increased intestinal permeability. A person with a leaky gut may experience a wide range of health conditions including IBS and food sensitivities (* , *).
One 2017 study found that supplementing with collagen peptides improves intestinal tight junctions, thereby reducing leaky gut (*).
For better gut health and overall health, choose a collagen peptide supplement that’s low-carb, made with grass-fed collagen, and doesn’t contain added sugars. You can try Perfect Keto’s high-quality collagen peptides.
What Foods Should Be Avoided with SIBO?
Allow your gut to heal by staying away from these foods that worsen SIBO symptoms:
- Sugar alcohols
- Dietary fat (limit your intake if you have SIBO with diarrhea)
- Laxatives (for SIBO with diarrhea)
- Cruciferous vegetables like broccoli and brussels sprouts (if you find that these foods give you gas and make you bloat)
- Processed foods in general
Keeping a food diary can be very helpful for identifying specific foods that contribute to SIBO symptoms. Based on your observations, you can create a keto low-FODMAP meal plan that works just for you.
What Happens If SIBO Is Left Untreated?
Untreated SIBO can lead to complications, which can range from mild or severe. Examples are nutrient deficiencies, malnutrition, weight loss, heart disease, bone disorders, and other health problems resulting from having too little nutrients (* , *).
A 2021 study published in the Journal of the American Heart Association noted a high prevalence of SIBO in patients with heart failure. Furthermore, SIBO led to rehospitalizations. This makes proactive even more important for heart failure patients (*).
If possible, work closely with a doctor who has successfully treated patients with SIBO, in addition to trying the natural remedies discussed earlier in this article.
When to See a Doctor and Testing for SIBO
SIBO signs and symptoms such as abdominal pain, bloating, flatulence, nausea, diarrhea, constipation, and unintentional weight loss need medical attention. Speak to your doctor if you experience one or more of these. Your doctor will perform a full evaluation and may order the following tests:
- Breath testing: This popular, non-invasive testing method checks for gases like hydrogen and methane exhaled by your lungs. However, while breath testing is easy and safe, it’s still possible to get false positive or false negative results (*).
- GI map stool testing: For a deeper assessment of your gut health, your doctor may order GI mapping, which detects gut microbes that produce certain gases. It also helps your doctor to check for low or high levels of beneficial and pathogenic microorganisms.
- Jejunal aspiration: While invasive and costly, a jejunal aspiration is more accurate. It involves aspirating a small amount of jenunal fluid (fluid from your jejunum, the second part of your small intestine) to test for bacterial overgrowth (*).
Conclusion
SIBO affects a person’s quality of life, especially with worsening symptoms. However, it can be easily diagnosed and treated with the help of a medical professional. Natural strategies such as following a keto diet for SIBO, eliminating FODMAPs, and taking probiotics for diarrhea will help ease symptoms.
Consider adding back a small amount of food from a FODMAP category once SIBO resolves to maintain a healthy and balanced microbiome. It also helps to document your symptoms, including your reactions to certain foods. If you’re experiencing persistent symptoms, don’t hesitate to reach out to your doctor.