Have your periods always been a little weird?
Does losing weight constantly feel like a never-ending battle against your own body?
Is your significant other sick of all the bathroom clutter from your acne washes and products to keep your excessive hair growth on the DL?
Though these strange and embarrassing occurrences may seem unrelated, if you’re dealing with them and you’re a female in your baby-making years, you could have PCOS.
Don’t be surprised if you haven’t heard of it.
Even though polycystic ovary syndrome (PCOS) is the most common endocrine disorder for premenopausal chicks and usually develops when you’re a teen, it’s estimated that almost 70% of sufferers don’t even know they have it[*].
Since PCOS is the number one cause of infertility in women, the diagnosis usually happens later in adulthood when you’re striving to get pregnant.
That means you could be dealing with the uncomfortable symptoms and dangerous health risk factors unknowingly your entire life.
Here’s the worst part: the medical world doesn’t know the exact cause of PCOS and no known cure exists.
And it gets worse.
Medications have traditionally been used to deal with the symptoms of PCOS, but they don’t solve the real underlying issue of why you have PCOS in the first place.
Now don’t rage against the medical community yet. Scientists are finally learning the connection between low-carb eating like the ketogenic diet and a reversal of PCOS symptoms.
That’s why we’ll be exploring the keto PCOS connection from the ground up today.
You’ll have answers to help explain topics like:
Whether you suspect you’re a PCOS cyster, you’ve been diagnosed and have tons of questions or you want to help a close lady struggling with it, this guide should give you everything you need to know about the keto PCOS link.
So let’s start by learning what PCOS does to your body.
PCOS and Your Body: Here’s What’s Going On
You know how you’re normally supposed to get a period every 28 days or so?
This happens because one of your ovaries releases an egg to get fertilized. During this process, a sac forms around the egg as it matures on the surface of your ovary. When the egg is released, the sac detaches and goes along for the ride.
You’ll either have that egg fertilized by determined sperm or you won’t get pregnant and your uterus will shed the womb it preemptively started for your future baby (i.e., you’ll get your period).
Or at least that’s how it should work.
When you have PCOS, your periods can be there one month and absent the next (if you even get them at all). That’s because your ovaries are experiencing egg release fails.
Instead of maturing and leaving the ovary nest, the unreleased egg continues to grow. Or if your egg is released during ovulation, the sac may stay behind, reseal and fill with fluid[*].
Either way you develop what’s known as a functional cyst.
Cysts are one of the classic signs you have PCOS: while a normal ovary will appear smooth on an ultrasound, an ovary affected by PCOS will have lots of small little bumps sprouted all over, which are those unreleased eggs as cysts built up over time.
You can thank a hormonal imbalance of too much luteinizing hormone (LH) and too little follicle-stimulating hormone (FSH) for this.
When your LH levels are high, your body starts producing too many androgens, or male hormones like testosterone.
Unsurprisingly, male hormones aren’t what your body needs to do girl things so they wind up suppressing ovulation (or the release of your egg) instead of helping.
Plus, since PCOS women have lower levels of sex hormone binding globulin (SHBG), there’s even more testosterone freely floating in their blood, which makes the situation much worse.
TL;DR: PCOS is a hormonal disorder that messes with your ovulation and causes irregular periods.
As a whole, PCOS was first formally introduced to the medical community in 1935[*] but the earliest published description of a woman with what we now recognize as PCOS was way back in 1721 in Italy[*].
Yet after all this time, scientists still don’t know the exact cause.
The accepted theory is developing PCOS takes a combination of genetics you can’t control and personal lifestyle choices which you can.
Genetic Factors Contributing to PCOS
PCOS is common in first-degree relatives though that doesn’t mean you’ll have it just because your mother or sister does.
PCOS has been attributed to a wide variety of triggers, such as[*]:
- Prenatal exposure to male hormones
- Excessive levels of male hormones
- Poor fetal growth
- Defects in insulin secretion
- Insulin resistance as a genetic adaptation
- Inflammation that causes polycystic ovaries to make excess male hormones.
Genetic abnormality that develops while you’re still in utero? Can’t do much about that.
So let’s talk about what you can change.
Almost 70% of women with PCOS have an increased risk of insulin resistance and glucose intolerance[*].
This is a big deal.
See, insulin is a hormone that helps control the amount of sugar (or glucose) that’s in your blood. It helps sugar get inside your cells so it can be used for energy.
When you have insulin resistance, your body doesn’t respond to the effects of insulin.
Insulin can’t get glucose into your cells so that sugar just hangs out in your bloodstream. Now you have high blood sugar. You could develop type 2 diabetes if this becomes a regular occurance.
So when you take your genetic predisposition for insulin resistance and add higher than normal insulin levels to the equation, you may trigger PCOS.
And high insulin levels don’t just happen overnight.
Unhealthy Lifestyle Choices Add Fuel to Your PCOS Fire
While being overweight may not specifically cause PCOS, 50% of women with this condition in the US are either overweight or obese[*].
Does being overweight cause PCOS or did PCOS cause you to become overweight?
Women with PCOS are naturally more insulin resistant and that makes losing weight and maintaining a healthy BMI the hardest struggle of your life.
You may be making this situation worse by increasing your body’s insulin (and insulin resistance) by doing things that raise your blood sugar, such as:
- Eating a high-carb or high-sugar diet
- Having more Netflix nights than gym days. When you don’t use all the glucose in your diet, it gets stored as fat around your tummy, liver and pancreas. This fat increases insulin resistance and male hormone production, creating a never-ending cycle[*].
- Stressing out. When you’re stressed and anxious, you raise your cortisol levels. This stress hormone amps up your body by releasing insulin so your cells have enough energy (glucose) to run away from danger. Only most of this stress is mental so your body never has the chance to burn all this off[*].
- Using products with hormone-disrupting chemicals such as BPA and parabens, which mimic the way hormones work in your body and confuse your body’s ability to regulate your real hormones, leading to imbalances and irregularities[*].
Ladies with PCOS who are also overweight are at an increased risk for scary health conditions including[*]:
- Type 2 diabetes
- Heart disease
- Hypertension, or high blood pressure
- Obstructive sleep apnea
- Coronary artery disease (CAD)
- Non-alcoholic fatty liver disease (NAFLD)
- Bleeding or cancer of the uterine lining
Plus, if you manage to get pregnant while your PCOS symptoms are left untreated, you’re at risk for:
- Premature birth or miscarriage
- Gestational diabetes
- High blood pressure during pregnancy.
That’s why your gyno’s first instruction is typically to lose weight if you’re above a healthy BMI.
Studies have shown that losing weight not only improves your good looks, it also lowers your male hormone levels and decreases your insulin resistance — two huge problems contributing to your PCOS[*].
Losing weight may also conveniently resolve a few other symptoms you’re dealing with as a result of PCOS.
Let’s get to those next.
The Signs and Symptoms of PCOS
The symptoms and side effects of being cursed with PCOS range from everything from menstrual irregularities to mood issues to losing weight.
Some of the most common include[*]:
Irregular menstrual cycles like having random periods (aka oligomenorrhea) and missed or absent periods (aka amenorrhea).
Infertility and trouble conceiving, because having irregular cycles makes it pretty hard to put a bun in the oven.
Weight gain and trouble losing weight, see the previous section on insulin resistance.
Multiple cysts on your ovaries that look like a “string of pearls” on an ultrasound. Not every woman with PCOS has cysts, but if you do have them, you’re more likely to have PCOS.
While most functional ovarian cysts shouldn’t cause much pain, you may develop cysts that grow large and painful or rupture. Then you’ll need serious medical attention.
“Masculine” features such as excess facial and body hair on your chest and tummy (aka hirsutism), thinning hair, male pattern baldness, acne… These are due to the extra male hormones floating around in your body.
Anxiety, panic attacks, mood swings, depression, fatigue and low sex drive may also be a result of your hormonal imbalances[*].
Acanthosis nigricans, or skin tags and darkened parts of your skin. Skin tags may appear in the folds of your armpits and neck. You may notice darker areas of your skin on your arms, groin and thighs.
You don’t have to suffer from all of these symptoms to have PCOS. According to the Rotterdam consensus, ladies must meet at least two of the following criteria to have PCOS officially:
- Infrequent or absent menstrual periods
- An excess or imbalance of sex hormones
- Polycystic ovaries confirmed via ultrasound
Because there’s such a gamut of what women experience under the PCOS umbrella, there are four main categories used to distinguish which type you may have[*]:
- Frank (or Classic) PCOS: infrequent periods, excess male hormones and polycystic ovaries (PCO)
- Ovulatory PCOS: excess male hormones, PCO and a regular menstrual cycle
- Non-PCO PCOS: infrequent periods, excess male hormones and normal ovaries
- Mild or Normoandrogenic PCOS: infrequent periods, PCO and normal level of male hormones
Now that you have a better idea of where you fall on the spectrum of PCOS — and you know the underlying reasons for it — you’re probably wondering how to get rid of it.
The best step you can take is to fight your body’s natural insulin resistance.
How can you do that?
You have to lose weight (if your BMI is too high) and you need to find a diet that ranks as low on the sugar scale as possible.
Drop a few pounds and remove all the excess insulin from your body and you may free yourself of all the symptoms and health risks we’ve been chatting about.
That’s what the ketogenic diet offers.
So let’s talk about the science behind the keto PCOS link.
How Does The Ketogenic Diet Treat PCOS?
Ketogenic diets have been around since the 1920s to treat patients with epilepsy. Now this way of eating is being studied for its potential to reverse diabetes, polycystic ovary syndrome, acne, and other conditions connected to insulin resistance[*].
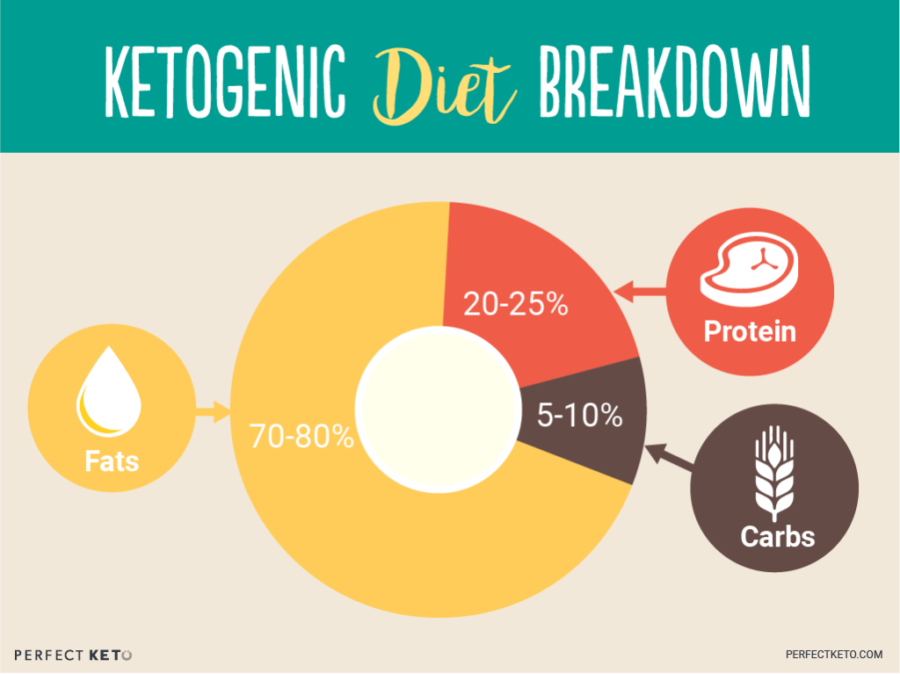
Unlike a traditional carb-rich diet, the ketogenic diet is a high-fat, moderate-protein and low-carb way of eating with the following macro breakdown:
Instead of your body using glucose for energy, a limited carb intake will switch your body to run on fat.
Your body is totally capable of functioning on fat for energy instead of glucose. It’s just easier for your body to use glucose when it’s available. Therefore, to get your body to run on stored body fat, you’ll need to deprive it of sugar.
Sure, glucose is a quick-digesting source of energy, but it’s so needy. When it runs low, it forces you to drop what you’re doing and give in to your craving for more sugar.
When your body becomes a keto-adapted, on the other hand, it will use up the fat from your diet and then start burning through your own fat stores for energy when it needs more.
Most ladies experience rapid weight loss like they’ve never experienced — just from switching to a keto diet alone.
Let’s talk about why this matters so much.
Lose Weight and Decrease Your Insulin Resistance
A low carb keto diet keeps you from eating foods that trigger insulin resistance and encourages weight loss. That’s why they’ve shown positive results in patients with type 2 diabetes and obesity, both of which are key in managing PCOS[*].
Because it takes your body longer to digest fat, you’ll feel fuller faster and for longer. You cut down your overeating and your tendency to graze for snacks[*]. Both of these are known diet saboteurs.
During one study, low carb dieters lost 14% of their body weight, reduced their insulin levels by at least 50% and lowered their insulin resistance and triglycerides[*].
That 14% drop may seem small, but on a 200-pound woman that’s losing 28 pounds! An achievement like this may be enough to tip your BMI out of the obese or overweight range and into healthier territory.
Even though PCOS women have a harder time losing weight, when 11 women with PCOS went keto for six months, they found similar results.
Ladies in this study lost an average of 12% of their body weight and dropped their fasting insulin levels by 54%[*].
Lower body weight and decreased insulin resistance may be enough to balance your hormones, silence your PCOS and even help you conceive.
Increase Your Chances of Getting Pregnant
Researchers from a recent overview of studies wanted to find out if a correlation between diet and fertility hormones exists in overweight and obese women.
They noticed significant improvements in reproductive hormones when women went on a low carb diet like keto six out of seven times[*].
They believed a low carb diet may not only improve hormonal imbalances so you can start ovulating regularly, but may also boost your chances of becoming pregnant compared to the usual carb-heavy diet.
And remember that study we just mentioned about the PCOS women crushing 12% of their body weight?
In that same study, scientists noticed the LH:FSH ratio improved across the board, which made it likelier for normal ovulation to occur. Maybe that’s why two of the women who had been struggling to get pregnant found luck and conceived before the study was over[*].
Banish Anxiety and Depression
Since anxiety and depression are both symptoms of PCOS, many girls are often prescribed drugs to combat these issues. But these may also lead to weight gain, furthering an already difficult process to lose weight and fight PCOS.
Keto may be used for depression.
In one study, PCOS women were split into two groups: one group followed a low-carb/high-protein diet while the other ate the traditional low-protein/high-carb diet.
After 16 weeks, the low carb women showed significant increases in their self-esteem and similar decreases in their depression. These changes were not observed in the high carb group[*].
So even though there’s technically no “cure” for PCOS, a low carb way of eating — and a ketogenic diet specifically — has been shown to be beneficial for lowering insulin levels, helping you lose weight and bettering your quality of life.
Are you finally ready to get started with one?
A Modified Diet for Keto PCOS
When you have PCOS, following a standard keto diet will work great initially, but you may need to make some minor tweaks and adjustments to see what works for your body.
After all, you’re not exactly “normal” and keto diets are still in their infancy of being studied for PCOS relief.
Follow these simple guidelines and you won’t complain when your PCOS symptoms start ghosting:
Find Your Carb Sweet Spot
Keto is all about restricting the amount of carbs you eat. While this works for many PCOS cysters, it might not work for you immediately.
See, if you’re used to eating most of your calories from carbs and you switch that fuel source off, your body may go into panic mode and ramp up insulin resistance even more.
So your first step is to figure out how many carbs you’re really eating.
Grab a food journaling app like MyFitnessPal and start plugging in what you eat on a daily basis to watch your macros add up. You may be shocked at first, but you need to know the truth.
A typical keto diet aims to keep daily carb consumption under the 30g mark.
If you’re eating close to 300g per day, this may be too drastic for your already sensitive system to handle at first.
Try starting out slow with 100g. Then move to 75g, 50g, 35g and maybe even 25g when you’re a seasoned low carb vet.
Listen to your body. If you need to add more carbs — say because you’re an endurance athlete and you can’t make it through your workouts — add them carefully in 5–10g increments to your daily net total.
Then when you’re feeling good, lower them again to see if your body adapts.
Though keto works best the fewer carbs you eat, you’ll still find success reducing your carb intake as much as you can.
When 24 women followed a low carb diet for eight weeks, they lost an average of 19 pounds and experienced significant reductions in their blood sugar levels, insulin resistance, triglycerides, and free testosterone levels — by simply limiting their net carbs to 70g per day[*].
Only you know how to find your sweet spot. Once you reach it you’ll have more energy than you ever had on the sugar train.
Treat Fiber Like Your BFF
Fiber not only helps control your insulin levels and ward off insulin resistance, it also keeps your digestive system running in smooth order, helps you feel full and reduces inflammation[*].
That’s why you should have at least 30g of fiber per day and aim for a bit of fiber with every meal and snack.
The best fiber sources for keto PCOS diets include:
- Avocado
- Cauliflower
- Broccoli
- Brussels sprouts
- Asparagus
- Bell peppers
- Chia seeds
- Flax seeds
- Dark, leafy greens (like kale, arugula and spinach)
Get Your Lignan Fix
Lignans are a type of fiber that may lower both your male hormone and insulin levels while also boosting your SHBG. Sounds like a keeper, right?
Lingnan-rich food sources for your keto PCOS diet include:
- Flax seeds
- Sesame seeds
- Berries
- Broccoli
In one PCOS study, women taking just one ounce of flax seeds each day noticed a dramatic decrease in their free testosterone levels[*].
Another showed that obese women consuming flax seeds had lower insulin levels and better insulin sensitivity than women who weren’t[*].
Fatty Fish and Nuts
Fatty fish like tuna, sardines, salmon, herring and mackerel contain healthy omega-3 fats, which have been studied for their ability to improve insulin sensitivity in ladies with PCOS and significantly decrease glucose, insulin, and insulin resistance[*].
And when 45 non-obese PCOS women were treated with omega-3 for six months, their sex hormones started to normalize and they improved both their hirsutism (excess body hair) and insulin resistance[*].
You’ll also find these powerful omegas in keto-friendly nuts. Both walnuts and almonds are beneficial at reducing androgen levels in women with PCOS[*].
So while you can’t change your genetics, a keto diet will help tremendously when it comes to managing your PCOS symptoms.
You should also follow these tips to round out your holistic PCOS treatment plan:
3 Extra Ways to Boost Your Keto PCOS Journey
While a keto diet may be enough to help you lose weight and stop your PCOS symptoms from taking over your life, you’ll notice the most success when you combine it with these three tips:
1. Exercise Daily
Exercise can help lower your blood sugar levels, prevent insulin resistance and support a healthy lifestyle. It’s also pretty crucial for losing weight and building fat-burning muscle too.
You should get at least 30 minutes of daily exercise. Science says both aerobic exercise and resistance training are perfect for women with PCOS:
When eight women with PCOS followed an aerobic exercise regime for 16 weeks, they noticed improved insulin sensitivity[*].
And if you’re suffering from missed periods or trying to get pregnant, aerobic exercise for 12 weeks in one study resulted in 56% of the participants restarting their menstrual cycle and 43% resuming normal ovulations[*].
Resistance training, on the other end of the spectrum, led to better reproductive function, lower androgens, and decreased visceral fat in a four-week study of 45 sedentary women with PCOS[*].
Yoga is another helpful form of exercise for PCOS cysters and may be able to improve insulin resistance, balance your hormone levels and lower your risk factors for heart disease[*].
Bonus: It’s also excellent for stress release.
2. Stress Less
Both anxiety and depression are complications of PCOS. But stress leads directly to being insulin resistant, which contributes directly to your PCOS symptoms.
So to lower those levels, you’ll need to level your head.
When 90 girls with PCOS practiced yoga and meditation for just one hour per day for 12 weeks, they had better blood sugar and insulin levels, more balanced sex hormone ratios, more regular menstrual cycles, and less hirsutism than girls who did not[*].
Plus, adding meditation to your yoga practice not only lowers your cortisol levels (so your body releases less insulin), it also banishes your stress and helps you sleep better.
3. Catch More Snooze Time
It’s hard for anyone to get a full eight hours of beauty rest, but researchers from one review found that “sleep disturbances were twice as common in women with PCOS compared with those without” it[*].
And women with PCOS also have greater difficulty falling asleep.
But PCOS women who skip a full night’s rest are at a greater increase for insulin resistance and menstrual irregularities[*].
So start logging seven to nine hours of sleep every night and put your phone to bed.
When you combine the insulin-lowering effects of a ketogenic diet with a daily exercise regime, methods to lower your stress and quality sleep, you’ll attack PCOS from all angles and increase your chances of reversing many of the causes and symptoms.
Keto Addresses the Root of PCOS
Unlike prescriptions used to mask what PCOS is doing to your body, a ketogenic diet addresses the main villain of the story (sugar!) so your ovaries can have the happy ending they deserve.
Women with PCOS have experienced easy weight loss, regular menstrual cycles, and greater luck conceiving just from switching to a low carb diet like keto.
So if you’re finally ready, check out the ultimate guide to starting a ketogenic diet now. Seriously, your ovaries need this.